RKP: Funktion & Erfolg
Das Rote Kreuz Österreich sammelt Rekonvaleszentenplasma. Das ist Blutplasma von Menschen, die COVID-19 überwunden und Antikörper aufgebaut haben, die helfen könnten, das Virus in anderen durch Übertragung von Plasma zu beseitigen.
Dies ist in mehreren Ländern derzeit ein Thema. Auch in England wurde angekündigt, dass NHS Blood and Transplant die Verwendung von Blut von Corona-Virus Überlebenden zur Behandlung von an der Krankheit erkrankten Patienten, untersuchen soll.
Dr. Lisa Lee Jones, Immunologie und Krebsbiologie, und Dr. Liliana Shalamanova, Immunologie und Nierenbiologie, an der Manchester Metropoliten University, UK, haben in diesem Artikel ihre Gedanken und Schlüsselfragen zur Funktionsweise der Therapie sowie die Erfolgschancen mit uns geteilt.
How will it work?
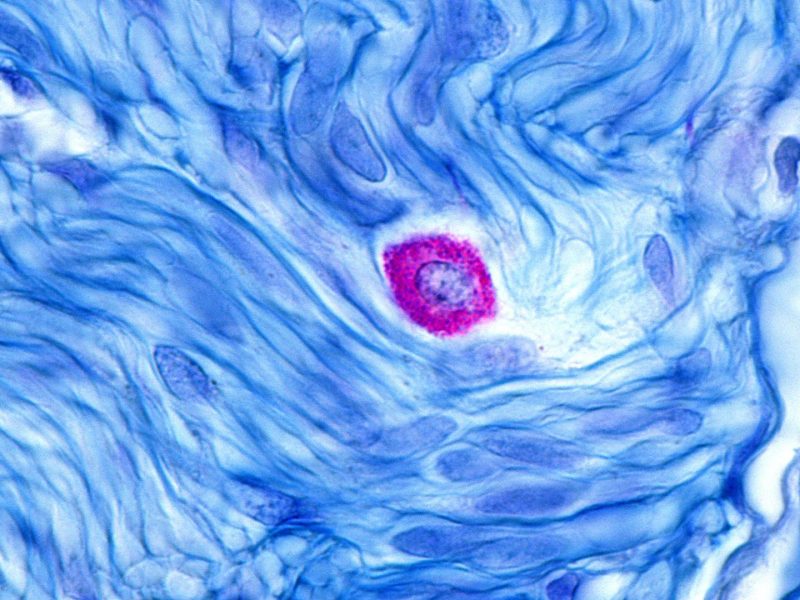
The immune system is designed to fight any germ we encounter during our lifetime. White blood cells provide an important role in our immune defence against germs, including viruses like COVID-19. One type of white blood cell produces molecules, called antibodies, in response to the germ a person has encountered. Antibodies are specific, so an antibody produced when somebody has the chicken pox virus will only attach to the virus that causes chicken pox, and not different germs, such as the ones that cause COVID-19.
Antibodies work in several ways: they can prevent viruses entering the body’s cells (effectively neutralising them), and also help them to be destroyed by special cells in the immune system. Antibodies are found in part of the blood known as plas- ma. Plasma is a straw-coloured liquid free of blood cells and accounts for about half of the volume of blood.
One of the treatments that is being explored to treat patients who are very ill with COVID-19 is to transfer plasma (and with it COVID-19 specific antibodies) from a patient who has already had it and recovered – known as convalescent plasma.
The transfer of antibodies is known as passive immunity and it provides temporary protection against a particular germ.
The reason for the temporary protection is that the amount of transferred antibodies is limited and they get used up over time. However, a transfer of convalescent plasma can buy time for the ill person and allow their own immune system to develop COVID-19 specific antibodies. Convalescent plasma transfer was used as an emergency treatment for COVID-19 in China and there is some evidence that it works. However, clinical trials are needed to determine the safety and effectiveness of this ap- proach. Two clinical trials in the UK are investigating the use of convalescent plasma. The Recovery trial, led by Peter Horby at the University of Oxford, will see if this treatment helps pa- tients recover before they are admitted to intensive care.
The Remap-Cap trial, led by the Intensive Care National Audit and Research Centre (ICNARC) in London, will investigate whether it will save patients who are already in high-dependency or intensive care units.
How many COVID-19 survivors would have to give blood to make this work and will all be able to supply useful amounts of antibodies?
The amount of convalescent plasma needed to support the recovery of a COVID-19 patient depends on the health-status of the recipient and on the concentration of the neutralising antibodies (antibodies which prevent the virus from entering their target cell) in the plasma of the donor. The levels of neutralising antibodies differ between donors, and they also de- pend on how soon after the recovery the plasma is donated. At present, we do not have robust data that show when the peak of COVID-19 antibodies is reached.
However, results from a previous SARS (Severe Acute Respi- ratory Syndrome) coronavirus clinical trial have shown that SARS-specific antibodies begin to increase three weeks after contracting the disease reaching highest levels at week 12.
Early data from a small study on neutralising antibody levels in COVID-19 survivors with mild symptoms suggest that middle aged (40-59 years) and older survivors (60-85 years) have significantly higher levels of neutralising antibodies than young survivors (15-39 years). Of note, not every COVID-19 survivor is a suitable plasma donor. The donors are selected based on age, weight, health status and their consent.
What kind of immune response is generated to a COVID-19 infection?
When someone is infected with a microbe, they produce lots of different antibodies to the same microbe. This is partly as a result of the process that generates diversity within the immune system to give it the capacity to deal with any pathogen we encounter in our lifetime, before we are even exposed to it. And it is also due to different antibodies produced to different parts of the microbe.
This antibody production is described as polyclonal, because there are lots of antibodies produced-and this is normal in an immune reaction.
When a patient is exposed to COVID-19, a polyclonal response would be produced, due to antibodies being raised against dif- ferent molecules present on COVID-19, and also different antibodies produced against different sections of one particular COVID-19 molecule. Therefore, there would be variability in the antibodies produced in different patients.
The commercial production of human monoclonal antibodies in the future would provide a standardised treatment, as is done for the treatment of other diseases such as cancer.
Could plasma therapy be used on all corona- virus patients or would it favour some profiles of patients better?
The timing of the plasma transfer in COVID-19 patients needs to be carefully considered. Ongoing clinical trials in the UK and around the world will soon provide reliable data on which patients benefit most from this therapy, and which is the optimal time to administer this therapy. Research also needs to be undertaken to determine why some people are more suscep- tible to the virus.
Clinical trials in SARS patients for example have shown that plasma therapy seems to be most effective in the early stages of the disease, especially in patients prone to severe virus-associated immune responses that lead to pneumonia.
The plasma therapy could blunt the severe response of the immune system by decreasing the abnormal release of particular molecules – the so called “cytokine storm” – which leads to severe inflammation. However, at present there are no tests which can determine who will develop severe inflammatory responses, so it is difficult to predict which patients will benefit most from plasma therapy. Plasma therapy may also be useful preventively for vulnerable groups such as those with pre-existing conditions, and those who are immunocompromised (such as cancer or autoimmune patients, and transplant recipients).
Are there any concerns about plasma therapy?
Plasma therapy could be life-saving. For example, it is used as a treatment in life-threatening snake and insect bites.
However, it may also lead to potential transfusion-related side effects such as serum sickness (hypersensitivity reactions), fever, chills, and over-reaction of the immune system.
Before transfusion the plasma is also tested for potential bloodborne infections such as hepatitis and HIV, to ensure that such infections are not passed on to the recipient.
Is the therapy guaranteed to work?
Passive immunity is effective for other conditions such as poisonous snake bites, and prevention of viral infections (such as cytomegalovirus). It was also used before antibiotics were introduced, to provide protection against tetanus and diphtheria. There has been renewed interest in passive immunisation due to bacteria becoming resistant to antibiotics.
The efficacy of plasma therapy depends on multiple factors, many of which are related to the age and health status of the recipient, and the stage and severity of their infection.
There is anecdotal evidence from China and USA that it works in COVID-19, however, it is important to await the clinical trial findings to determine whether plasma therapy is safe and effective for this disease.